The shortage of healthcare professionals is a concern in many countries, directly affecting the quality of healthcare services. Estonia has also set a goal to increase the number of educational slots for healthcare professionals. Haap Consulting conducted a study commissioned by the Ministry of Social Affairs, aiming to find suitable methods of compensating clinical supervision based on international practices.
In the 2021/2022 academic year, slightly over 500 nursing students were enrolled, while this year the plan is to admit 700 interested individuals. The number of slots in other specialist disciplines is being increased from the current 126 to 200. In this regard, starting from 2024, the Ministry of Social Affairs will cover the costs associated with the clinical practice of nursing and other priority healthcare professionals’ applied higher education.
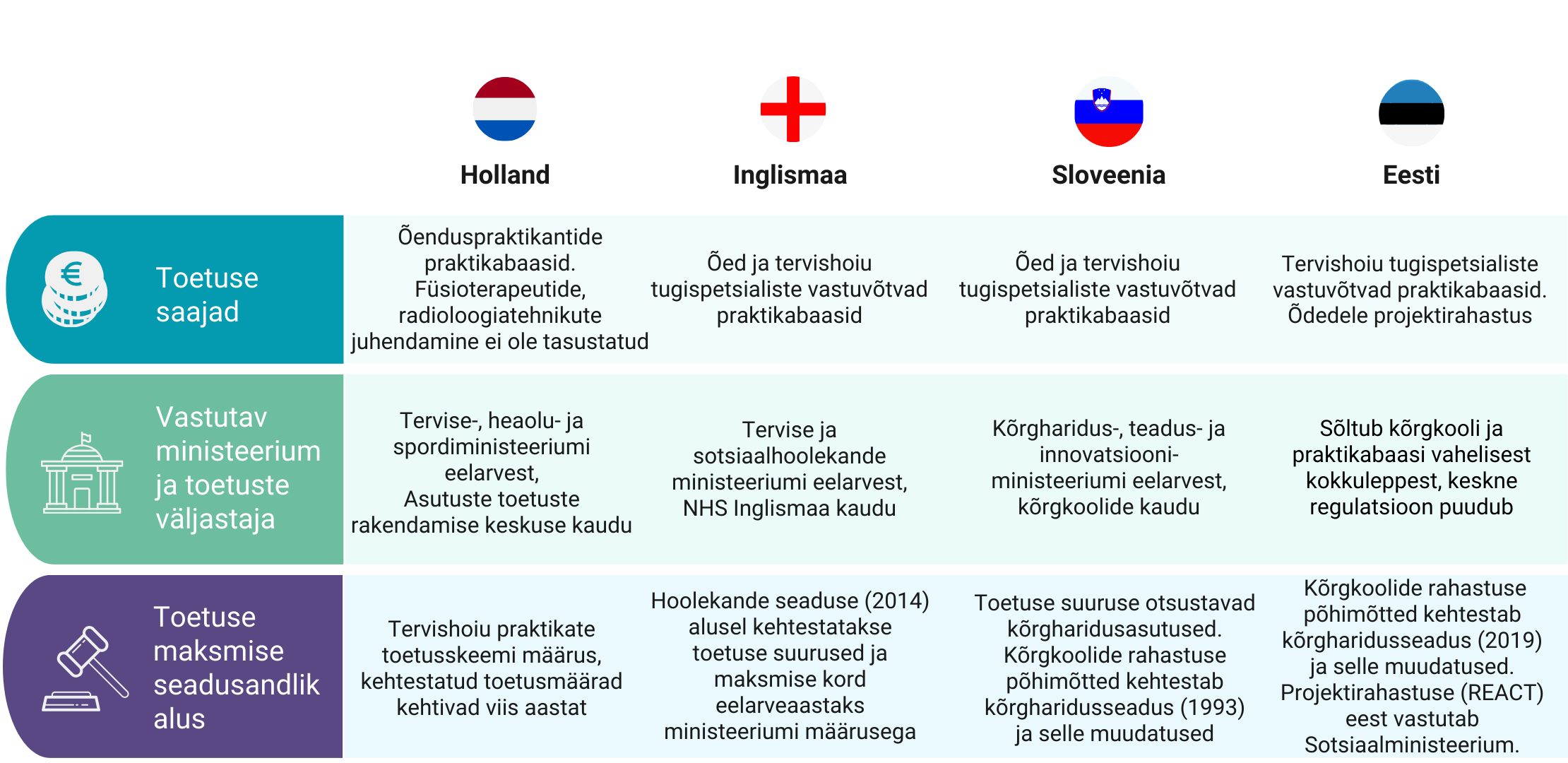
The analysis compared the experiences of three foreign countries – the Netherlands, the United Kingdom (specifically England), and Slovenia – in organizing and funding the clinical practice of healthcare professionals. To supplement the analysis of these countries, we conducted focus group discussions with Estonian professionals, involving professional associations, healthcare institutions, policymakers, and students. Besides financial compensation, the analysis also addressed the broader organization of clinical practice, including support for the work organization of clinical supervision.
The analysis of the current situation in Estonia revealed that the existing system of clinical practice organization is not sufficiently motivating for supervisors and practice bases. Clinical supervision is predominantly unpaid or for a symbolic extra fee (up to €1/hour), and there is no regulation or funding to standardize compensation for supervision. In addition, the organization of clinical practice varies between educational institutions and practice bases, complicating planning and leading to disparities in students’ clinical experiences.
The analysis resulted in the following recommendations and an initial action plan to support their implementation:
Goal: Increasing the number of clinical placements
1.1 Creation of a national capitation system for practice bases
1.2 Additional funding for practice bases that significantly increase the number of available clinical placements
Goal: Standardizing clinical practice management
2.1 Standardizing organizational issues with the help of the healthcare professions’ training commission
2.2 Creation of clinical practice coordinators’ roles in hospitals
2.3 Creation of a responsible supervisor role in hospitals
2.4 Creation of a unified information system
Goal: Supporting supervisor motivation
3.1 Central funding of additional payments for clinical supervisors
3.2 Valuing the position of a clinical supervisor
Goal: Ensuring the quality of supervision
4.1 Supporting the training of clinical supervisors
4.2 Conducting annual feedback surveys and communicating the results to practice bases
4.3 National recognition of practice bases that meet quality criteria
Goal: Supporting the learning opportunities of the trainee
5.1 Clinical practice scholarship